Fighting Drug Resistance in Colorectal Cancer with a Triple Attack!
Despite recent genomics-driven advancements in drug discovery and introduction of novel therapeutics, colorectal cancer (CRC) remains the fourth most commonly diagnosed and third most deadly cancer worldwide [1]. Five-year survival prognosis is highly dependent on the stage of the disease, with 90% survival rates for stage I dropping to barely 10% by stage IV metastatic CRC (mCRC) [2].
These poor survival rates are due to acquired drug resistance, in which patients responding positively to initial treatment begin to relapse as their tumours adapt and regrow. Effective first line therapy is a key determinant of patient outcome, with RAS and BRAF representing important biomarkers when determining the choice of therapeutics [2].
Identification of the mutations which activate receptor tyrosine kinases and downstream pathways in CRC led to the development of therapeutic kinase inhibitors. Unfortunately, in comparison with expectations, these have underperformed in clinical studies due to the complex cross talk and feedback among signalling pathways; targeting one point leads to pathway reorganisation and cancer cell survival [3].
Combined inhibition of different kinases and pathways is a recent, more effective approach, especially when pairing chemical inhibitors with other techniques such as angiogenesis inhibitors and EGFR blocking antibodies. Clinical trials in the Netherlands with active BRAF-driven CRC showed that the use of a three-target approach of MAP and MEK kinase inhibitors, together with the EGFR-blocking antibody Cetuximab, led to improved results [4].
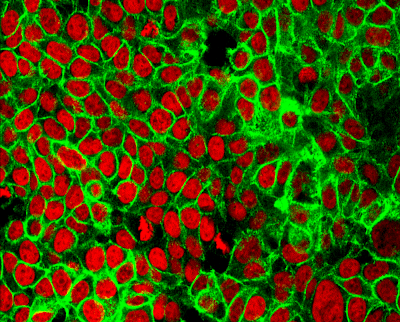
Well-characterised in vitro models are required to test putative drug combinations in clinically relevant models with genetically defined backgrounds. A promising study carried out by Dr Paul Clarke at the ICR showed that, in a panel of 47 CRC cell lines, a ‘triple attack’, with inhibitors of MEK and PI3Kα/δ kinases alongside low concentrations of an apoptosis-inducing BCL2 family inhibitor, improved the synergistic interaction of these compounds and blocked the acquisition of drug resistance in these models [6].
In vitro data generated from 2D cancer models has traditionally driven the journey to the clinic. However, studies validating the predictive nature of patient-derived cancer organoids show that these models mirror the in vivo reality much more closely than 2D models [7], likely because they more faithfully preserve tumour architecture and heterogeneity. Patient-derived organoids therefore represent a step towards predictive compound screening, and the designing of drugs that underpin the next generation of better performing CRC combination therapies.
1. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019; 14(2): 89–103.
2. Drug resistance and new therapies in colorectal cancer World J Gastroenterol. 2018 Sep 14; 24(34): 3834–3848.
3. Targeting Receptor Kinases in Colorectal Cancer Cancers (Basel). 2019 Apr; 11(4): 433.
4. Encorafenib, Binimetinib, and Cetuximab in BRAF V600E–Mutated Colorectal Cancer, New England Journal of Medicine (2019). DOI: 10.1056/NEJMoa1908075
5. Colorectal Cancer in Europe: A framework for Improving Outcomes for Patients 2020
6. Paul A. Clarke, et al. Dissecting mechanisms of resistance to targeted drug combination therapy in human colorectal cancer. Oncogene (2019) DOI: https://doi.org/10.1038/s41388-019-0780-z
7. Bartfeld S, Clevers H. 2017. Stem cell-derived organoids and their application for medical research and patient treatment. J. Mol. Med. 95: 729–38
