In the vast pharmacopeia of pain relief medications, one name stands out for its ubiquity and effectiveness: ibuprofen. Whether it's soothing a headache or a hangover, easing period pains, alleviating muscle aches, or reducing inflammation, ibuprofen has become a household staple and “a bedrock of pain relief and fever treatment all over the world.” But how did this wonder drug come to exist, and what does the future hold for it?
Ibuprofen: origins and history
In the 1950s and 1960s, pharmaceutical researchers were on a quest to develop safer alternatives to existing pain relief medications synthesised from salicylic acid, notably aspirin. Despite their effectiveness and versatility, these compounds came with gastrointestinal side effects that limited their widespread use - including stomach irritation, ulcers, and bleeding.
The breakthrough came somewhat serendipitously in the 1960s, when British pharmacologist Stewart Adams and his team at Boots Pure Drug Company were looking for a cure for rheumatoid arthritis (RA). At the time, aspirin was the preferred treatment for RA, but often needed to be prescribed in large doses that risked serious side effects. Adams began by studying how aspirin worked, hoping to find a compound that mimicked its anti-inflammatory qualities, but without unpleasant complications. He and chemist John Nicholson tested more than 200 compounds derived from salicylates, although none proved superior to aspirin – going on to study hundreds of other candidates over several years before deciding to investigate propionic compounds. Eventually, they synthesised ibuprofen, a ‘trivial name’ derived from fragments of the compound’s scientific name, (±)-2-(p-isobutylphenyl)propionic acid. Ibuprofen was granted a British patent in 1964, and proved successful in clinical trials on RA patients two years later. In 1969, it was approved as Brufen – a prescription drug for RA.
In time, however, ibuprofen’s wide-ranging benefits became more generally known: a process helped along somewhat unconventionally when Adams himself took 600mg of the drug while suffering from a vodka hangover in Moscow, where he was due to deliver an important speech at a pharmacological conference. “He took a handful of ibuprofen and felt fine. No hangover!” Adams’ son David later told the Smithsonian Magazine. Somewhat poignantly, Adams would regard the success of ibuprofen as a pain relief medication with some regret, given that the drug could help with symptoms of RA but not reverse them. “My father was enormously proud of what he accomplished, but readily admitted that it was based on a failure,” said David Adams.
Ibuprofen becomes a global success
If Adams felt ambivalent about the success of his invention, the rest of the world had fewer doubts. After proving effective in treating non-rheumatic conditions, ibuprofen was approved as an over-the-counter pain reliever in the United Kingdom in 1983 (as Nurofen) and soon after in the United States (as Advil). By 1985, when Boots’ worldwide patent expired and generic versions became available, more than 100 million people in 120 countries had used ibuprofen, which also earned its developers a Queen’s Award for Technological Achievement in the UK the same year. Even in 2021 - more than 50 years after it was first approved, and despite also being widely available over the counter - ibuprofen was still the 36th-most commonly prescribed medication in the United States. Today, it’s estimated that one pack of ibuprofen is sold every three minutes in the US.
Adams also received a number of personal accolades related to ibuprofen – including becoming an officer of the Order of the British Empire in 1987, and (with Nicholson) being inducted into the American National Inventors Hall of Fame. But perhaps the most heartfelt accolade arrived in 2007, when The Observer included him on a list of ‘The 50 Men Who Really Understand Women’ - “Because he discovered the wonder drug RD 13621, better known as ibuprofen, and the most effective remedy for hangovers and period pain known to womankind.”
Ibuprofen: side-effects
According to the world authority on ibuprofen, Professor Kim Rainsford, Adams’ brainchild has been so successful because “It is handled and metabolised in the body very predictably. It accumulates very well in sites where you need pain relief (and) it's got a very good safety profile...” However, like all drugs, ibuprofen does have certain side-effects, with the more common including headaches, nausea and indigestion. The drug is also associated with an increased risk of heart disease and stroke, as well as renal damage and gastric bleeding, particularly for those who consume it for extended periods and/or in higher doses.
Ibuprofen mechanism of action, synthesis and impurities
For the very last word in ibuprofen chemistry - including common synthesis routes, impurities, degradation products and mechanisms of action, download our free and exclusive poster here, and watch the accompanying video below.
The ‘great promise’ of ibuprofen, nanotechnology and personalised medicine
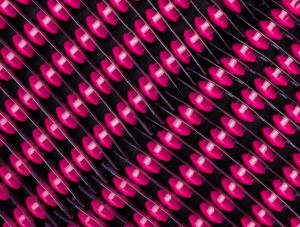
By any standards, ibuprofen is a mature medicine. But its therapeutic potential is far from exhausted. As one recent review of preclinical research puts it, ibuprofen and other Non-Steroidal anti-inflammatory drugs (NSAIDs) still have “great promise”, thanks to advances in drug delivery systems such as nanotechnology, as well as improvements in personalised medicine.
The clinical performance of NSAIDs like ibuprofen can benefit from nano-drug delivery in various ways. These include redirecting the drug from normal tissues towards critical sites, thus significantly reducing the dose required, and therefore lowering the risk of toxicity. Solid Lipid Nanoparticles (SLNs) loaded with matrix lipids such as stearic acid, tripalmitin, and trilaurin have also been shown to increase ibuprofen’s solubility, and thus its bioavailability and effectiveness. Furthermore, in pre-clinical experiments on rats, delivering ibuprofen sodium via a gelatine nanoparticle improved the drug's plasma half-life. All of which means that, in future, people taking ibuprofen for chronic conditions can hope to do so less frequently, with more rapid onset of pain relief, and with fewer side-effects.
The growing focus on personalised medicine, based on each person’s unique genetic makeup, may meanwhile be opening up exciting new avenues for tailoring ibuprofen therapy to individual patients. Techniques such as genetic profiling and biomarker analysis may help identify patients who are most likely to benefit from ibuprofen and predict their response to treatment. This precision medicine approach could also optimise dosing regimens and minimise adverse reactions, maximising the drug's therapeutic potential.
Perhaps one day, our greater knowledge of each individual’s unique genetic composition may help us find effective cures for some of nature’s most stubborn diseases – including rheumatoid arthritis, Stewart Adams’ original and as yet undefeated adversary? Researchers from The Jackson Laboratoryhave explained the genomic basis of why some patients did not respond as expected to the leukaemia drug Gleevec, and also identified a drug that can be used in combination with it to potentially help these individuals. Could a similar approach help to complete Adams’ work and find a combined treatment regime that reverses RA – with ibuprofen fittingly part of the mix?